Depression is a major mood disorder that affects more than 264 million people across the globe and ranks as the leading cause of disability worldwide. Even more alarming, the problem seems to be steadily increasing among people of all ages, particularly teens and young adults.
Besides being seriously debilitating, major depression often comes with a grave side effect — thoughts of suicide that can lead to attempted suicide without timely intervention and help.
At Bespoke Treatment in Los Angeles and Santa Monica, California, we know that traditional depression treatments have helped many people find lasting symptom relief. But we also know that the conventional approach doesn’t work for everyone, and it doesn’t always deliver the kind of rapid relief that’s most needed in times of major distress.
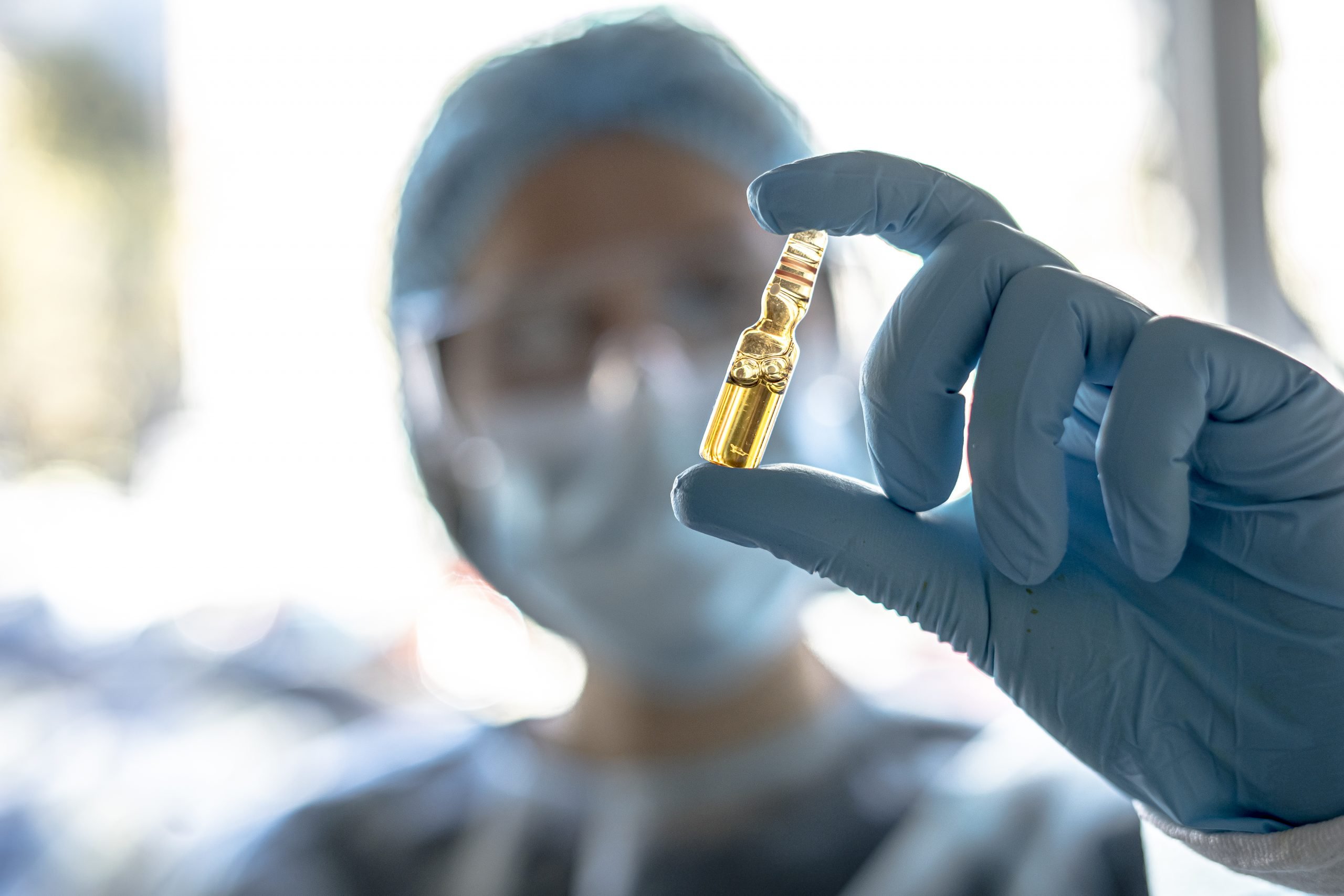
That’s where ketamine comes in. Find out how this fast-action treatment for major depression has become a game-changing solution for the patients who need it the most.
A brief history of ketamine
Ketamine isn’t a new medication — in fact, it was first synthesized more than half a century ago in 1962, when it was initially used as an anesthesia for minor surgery. Following its approval by the U.S. Food and Drug Administration (FDA) in 1970, it quickly became the most widely used battlefield anesthetic in the Vietnam War.
As the 1970s continued, veterinarians realized that ketamine was also safe and effective for animals; by 1985, its widespread use in medicine (internal, pediatric, and veterinary) earned it a spot on the World Health Organization’s (WHO) list of essential pharmaceuticals.
At this point, the story of ketamine veers a bit off course… into the world of illicit drug use. Its popularity as a recreational substance was especially prevalent among partygoers, who sought out its immediate and dissociative effects.
Then, in the early 2000s, as psychopharmacology experts struggled to find a more effective antidepressant that wouldn’t lose efficacy, researchers began exploring ketamine as a possible solution.
The problem with conventional antidepressants
All conventional antidepressants target similar mechanisms in the brain to alleviate symptoms — they increase the activity of a class of neurotransmitters called monoamines, which includes serotonin, norepinephrine, and dopamine.
These medications must build up in your system before they’re effective, and they don’t always remain fully effective over time. Research shows that decreased drug efficacy (tachyphylaxis) affects about 25% of people who take selective serotonin reuptake inhibitors (SSRIs), the most commonly prescribed antidepressants.
While experts don’t know exactly why these medications lose their effectiveness over time, it’s thought that the targeted brain receptors become less sensitive (i.e. more tolerant) to the drug.
As soon as this predicament became evident in the 1990s, researchers began searching for a way to improve conventional antidepressants. Their lack of success prompted them to look for a new type of antidepressant — one that targets mechanisms beyond monoamines.
The promise of ketamine: a new approach to depression
That’s when researchers began asking what would happen if they could target glutamate, the all-important excitatory neurotransmitter that helps “turn on” the key brain circuits that drive all forms of behavior.
After studying the effects of altered glutamate neurotransmission in healthy people as well as schizophrenic patients, researchers figured out that a glutamate receptor blocker (antagonist) called ketamine had major psychological effects, inducing psychotic symptoms.
With the understanding that glutamate plays an important role in mood regulation as well as the regulation of monoamines, researchers began to wonder if lower doses of ketamine could be used to alleviate depression.
Indeed, they discovered that low-dose ketamine infusions — much lower than the amount that produces psychotic symptoms — produced a surge of glutamate transmission in the brain that could reduce depressive symptoms quickly and dramatically, usually within a few short hours.
An ultra-rapid shift in cognition and mood
Experts are still trying to figure out exactly how ketamine causes such a rapid cognitive shift, even in patients who suffer from treatment-resistant depression (TRD). Current research shows that it appears to induce changes in brain circuit function first, causing depressive symptoms to subside within hours.
It also appears to stimulate the regrowth of synapses between neurons, promoting increased connectivity between neurons that fosters increased activity in the regions of the brain that are most subdued by depression.
Recently, researchers have discovered how ketamine appears to affect such a rapid change in cognition and mood at the molecular level. Your brain cells contain guanine nucleotide-binding proteins (G proteins), a special family of proteins that act as molecular switches. G proteins help carry messages from outside the cell to its interior.
People with depression tend to have an abnormally high number of inactive G proteins stored on “lipid rafts” within their cellular membranes. Regular antidepressants gradually accumulate on these lipid rafts, ultimately forcing the G proteins off their resting spot and back into action.
Ketamine, on the other hand, pushes inactive G proteins off their lipid rafts much more quickly (often in minutes), and keeps them active for a longer period of time following treatment.
Besides being a highly effective treatment for depression and suicidal ideation, ketamine can be used to help alleviate anxiety, post-traumatic stress disorder (PTSD), and chronic pain.