PTSD is a debilitating disorder that can arise after experiencing or witnessing a traumatic event. The traditional treatments for PTSD typically include psychotherapy and medication, but they don’t work for everyone. This has led to a growing need for innovative treatment options. Ketamine therapy for PTSD represents a breakthrough, providing new hope for patients struggling with persistent and severe symptoms. Its ability to potentially reset certain neural pathways offers a different approach from conventional methods, highlighting the importance of innovation in mental health treatments.
How Ketamine Treats PTSD
Mechanism of Action
Ketamine acts uniquely compared to traditional medications used in PTSD management by targeting the glutamate system in the brain. Glutamate is the most abundant excitatory neurotransmitter, involved in almost every major brain function, including cognition, memory, and learning. Ketamine for complex PTSD works by blocking certain receptors in the glutamate system, which can help alleviate symptoms by reducing the hyperactivity in the brain that is often associated with PTSD.
Impact on Mood Regulation and Cognitive Function
One of the critical benefits of ketamine infusion for PTSD is its rapid impact on mood regulation and cognitive functions. Patients often report a significant uplift in mood shortly after treatment, which is crucial for those suffering from severe depressive episodes linked to PTSD. Moreover, ketamine has been shown to enhance cognitive flexibility, helping individuals break free from the rigid patterns of negative thinking that are typical in PTSD. This improvement in cognitive function is vital for effective engagement with psychotherapeutic treatments and better overall mental health.
Resetting Neural Pathways
Ketamine for post-traumatic stress is thought to ‘reset’ neural pathways by promoting the growth of new synapses. This ability to create new neural connections can help patients overcome entrenched patterns of behavior and thought that contribute to the persistence of PTSD symptoms. The resetting process is particularly beneficial for those with treatment-resistant forms of PTSD, offering a chance to respond better to psychological interventions after undergoing ketamine therapy.
The Process of Ketamine Therapy for Trauma
What to Expect During Ketamine Infusion Sessions
During a ketamine infusion for PTSD, the treatment is administered intravenously in a controlled clinical setting. Patients are closely monitored by healthcare professionals throughout the session, which typically lasts between 40 to 60 minutes. During the infusion, patients might experience altered perceptions, such as heightened sensory sensitivity and changes in the perception of time, which are temporary and subside quickly after the session ends. To help create an atmosphere that’s supportive of the treatment’s benefits, the environment is frequently constructed with quiet areas and low lighting.
Frequency and Duration of Treatments
Ketamine treatments for PTSD represent a promising approach, leveraging its rapid-acting effects to alleviate symptoms. The regimen for administering ketamine is tailored to suit the specific requirements and responses of each patient, which can vary significantly based on individual health conditions and the severity of symptoms. Typically, a standard course of treatment involves:
- Initial Treatment Phase: This phase includes an initial series of infusions that are typically administered over two to three weeks. The objective during this phase is to quickly establish a level of ketamine in the body that can start to reduce the symptoms of PTSD. Patients often receive a total of six sessions during this time, each designed to progressively build upon the last, helping to establish a foundation for symptom relief.
- Maintenance Therapy: Following the initial series, maintenance infusions are introduced. These sessions are scheduled less frequently and are based on the patient’s ongoing response to treatment. The purpose of maintenance therapy is to sustain the benefits achieved during the initial treatment phase while adapting to the patient’s long-term needs. This might involve infusions every few weeks or months, tailored to maintain stability and prevent relapse.
By customizing the frequency and duration of ketamine treatments, healthcare providers aim to offer a therapy that adapts to the changing needs of patients with PTSD. With greater results and an improvement in general well-being, this strategy helps guarantee that every person receives the most suitable degree of care.
Monitoring and Safety During Treatment
Clinics offering this treatment are equipped with advanced monitoring equipment to track patients’ vital signs and overall well-being during each session. Medical staff are trained to handle any immediate side effects and ensure the patient’s comfort and safety throughout the process. Regular follow-ups and assessments help to measure the treatment’s effectiveness and make necessary adjustments, ensuring that each patient’s course of therapy remains safe and beneficial.
Post-Treatment Effects and Care
After a ketamine session, patients may feel immediate improvements in their PTSD symptoms, including reduced anxiety and a more positive mood. However, PTSD relief with ketamine can vary in duration. To maximize the benefits and maintain symptom relief, patients are advised to participate in additional therapeutic activities such as counseling or cognitive-behavioral therapy.
Benefits of Ketamine for PTSD
Rapid Symptom Relief
Unlike traditional antidepressants that may take weeks to become effective, ketamine can begin to alleviate symptoms within hours of the first infusion. This quick action can be crucial for individuals suffering from intense, debilitating symptoms, offering an immediate sense of relief and a potential reduction in the risk of self-harm or severe depression.
Mental Health Outcomes
Ketamine infusion for PTSD not only targets specific symptoms but also contributes to overall mental health improvement. Patients report enhanced emotional stability, better sleep patterns, and increased ability to engage positively with others. These broader benefits are vital for long-term recovery, helping individuals rebuild their lives and improve their quality of life following traumatic experiences.
Formats of Ketamine Treatment for PTSD
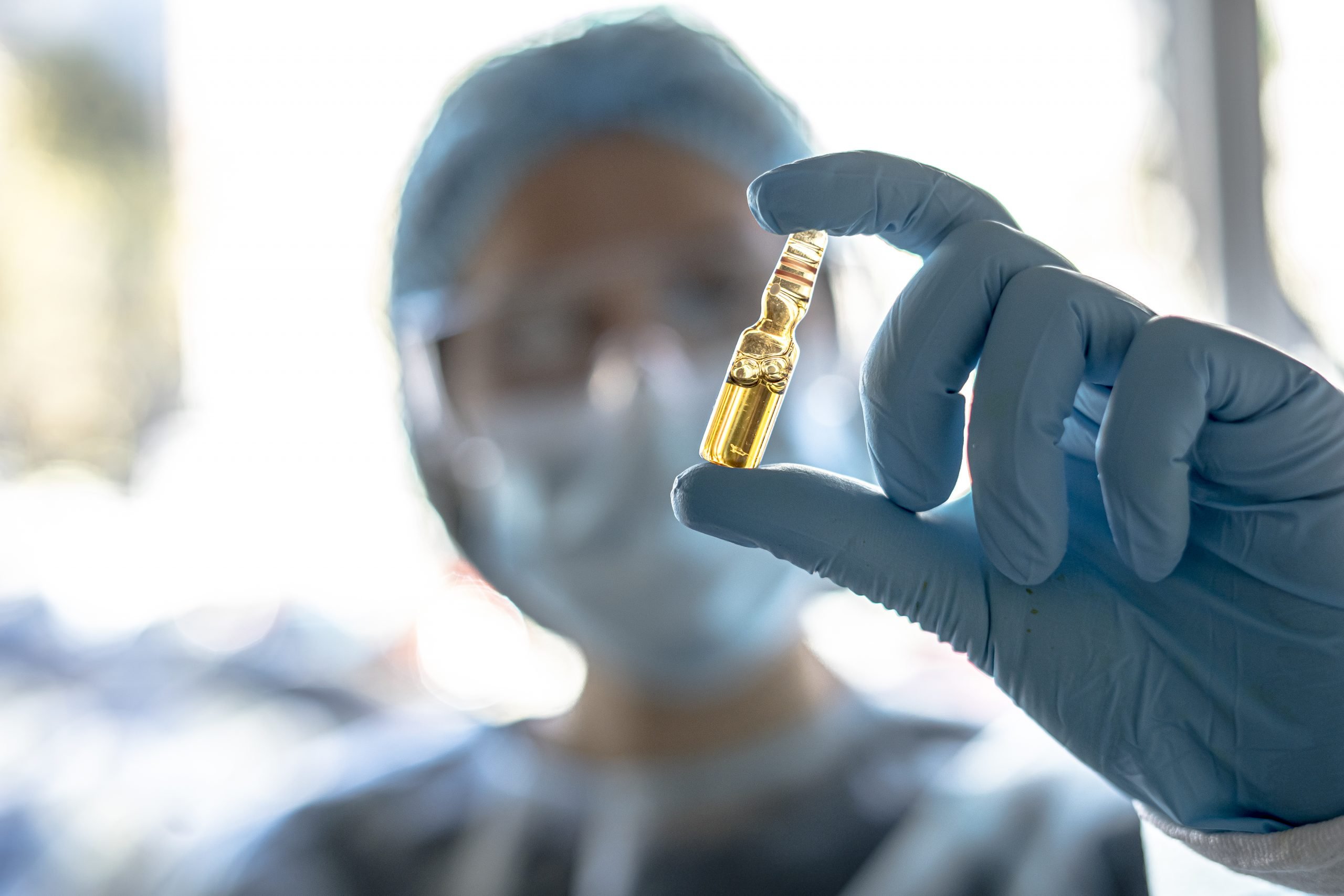
Intravenous Infusions
Intravenous (IV) infusion is the most common method of administering ketamine for PTSD treatment. This procedure involves delivering ketamine directly into the bloodstream through a vein. The benefits of this method include precise control over the dosage and immediate absorption, allowing for quick symptom relief. IV infusions are generally performed in a clinical setting where medical professionals can monitor the patient’s response in real time, adjusting the dose if necessary to maximize efficacy while minimizing side effects.
Intranasal Applications
It is another format available for treating PTSD. As an alternative to IV infusions, this technique includes using a nasal spray to administer a ketamine solution. It is more convenient and less intrusive. The benefits of intranasal ketamine include ease of use and the ability to administer the treatment in a variety of settings, potentially even at home under professional supervision. This method still offers a rapid onset of effects, though the bioavailability and dosage precision can vary more than with intravenous delivery.
Finding Reputable Ketamine Clinics
Identifying Certified Practitioners and Clinics
When seeking ketamine treatment for PTSD, it’s important to choose a clinic that employs certified practitioners. Certification ensures that the professionals administering the treatment have undergone the necessary training to safely and effectively deliver ketamine therapy. Patients should verify the credentials of the clinic and its staff, as well as check for reviews or testimonials from previous patients to measure the quality of care provided.
Cost Implications of Ketamine Therapy
The cost of PTSD ketamine treatment can vary widely depending on the clinic, the number of sessions required, and whether additional support services are included. While some insurance plans may cover parts of the treatment, many patients will find themselves facing significant out-of-pocket expenses. Transparent discussion with the clinic about the expected costs and payment options is essential to avoid unexpected financial burdens.
Navigating Insurance Coverage
Insurance coverage for ketamine infusions for PTSD is still limited. However, some insurance companies may cover the treatment under certain conditions or for off-label use. Patients should consult with their insurance provider to understand the specifics of what is covered and any prerequisites for reimbursement, such as a referral from a mental health professional or documentation of previous treatment failures.
Tips for Choosing the Right Clinic
Beyond basic criteria like cost and certification, several nuanced factors contribute to a clinic’s suitability. These factors include treatment customization, side effect management, continuity of care, interdisciplinary collaboration, and the therapeutic environment. A well-rounded assessment of these elements can lead to better treatment outcomes.
- Personalized Therapy Plans: Effective ketamine therapy requires a tailored approach, considering the unique psychological and physiological aspects of each patient. Check if the clinic assesses individual backgrounds, symptoms, and treatment histories to create personalized therapy plans. This level of customization should include adjustments based on patient feedback and progress throughout the treatment process, ensuring that the therapy evolves with the patient’s changing needs.
- Follow-up Care: A good clinic will offer comprehensive follow-up services, which should involve regular check-ins, support groups, and access to mental health professionals. These follow-up services help integrate the therapy into the patient’s overall treatment plan, contributing to long-term stability.
- Collaboration with Mental Health Providers: PTSD often requires a multifaceted treatment approach. Opt for a clinic that values and facilitates coordination with your existing mental health care providers. This collaboration should aim to create a seamless care continuum, ensuring that all professionals involved are informed and engaged in the treatment process, which can enhance therapeutic outcomes and patient well-being.
- Environment and Staff: The setting of the clinic and the approachability of its staff play pivotal roles in the therapy’s success. A warm, welcoming environment, coupled with empathetic, knowledgeable staff, can make a significant difference in a patient’s comfort and confidence in the treatment. Assess the clinic’s environment and interact with the staff before committing to treatment to ensure it feels supportive and conducive to healing.
When making your decision, it’s beneficial to visit the clinic, speak to the staff, and possibly connect with past patients. This comprehensive evaluation ensures that the clinic not only meets technical standards but also aligns with your personal needs and treatment goals, enhancing the likelihood of a positive therapeutic experience.
Integrating Ketamine Therapy with Other Treatments
Cognitive-behavioral Therapy (CBT)
CBT focuses on changing negative thought patterns and behaviors, which complements the biochemical effects of ketamine on the brain. When used together, ketamine can provide rapid symptom relief, allowing patients to engage more effectively in CBT by reducing barriers like acute anxiety or depression. Such a combination can accelerate recovery, helping patients develop healthier coping mechanisms and more resilient mental frameworks.
Enhancing Outcomes with EMDR
Eye Movement Desensitization and Reprocessing (EMDR) is another therapeutic technique that can be combined effectively with ketamine therapy. EMDR helps patients process and integrate traumatic memories, a process that can be significantly enhanced by the neuroplastic effects of ketamine. When used concurrently, ketamine’s ability to foster a receptive brain state may deepen the therapeutic impact of EMDR, leading to more profound and lasting healing from trauma.
Ongoing Research and Broader Applications
Exploring Ketamine’s Potential
Research into ketamine’s potential does not stop with PTSD; ongoing studies are investigating its effects on a variety of other mental health conditions, including severe depression, anxiety disorders, and bipolar disorder. Preliminary results are promising, indicating that ketamine may help fill treatment gaps left by traditional therapies. Its ability to rapidly alleviate symptoms and promote neuroplasticity could revolutionize treatment paradigms across the spectrum of mental health disorders.
Future Directions in Ketamine Research
The future of ketamine research involves not only expanding its applications in mental health but also refining treatment protocols to enhance safety and efficacy. Continued studies aim to determine optimal dosing schedules, minimize potential side effects, and identify which patient populations can benefit most from ketamine therapy. Researchers are also exploring how ketamine can be combined with other drugs or therapeutic modalities to further enhance its therapeutic potential.
Emerging Trends and Innovations
The landscape of ketamine therapy is continually evolving, driven by technological advancements and deeper scientific understanding. Innovations in delivery methods, such as wearable devices for controlled dosing or new formulation types, are on the horizon. These developments aim to make ketamine therapy more accessible and tailored to individual needs, potentially transforming the approach to mental health treatment globally.
For those considering ketamine for PTSD treatment, it is crucial to make informed decisions based on a comprehensive understanding of the treatment’s benefits and risks. Prospective patients should seek out accredited clinics, engage with knowledgeable healthcare professionals, and consider the financial aspects and potential insurance coverage. Awareness and education are key to maximizing the positive outcomes of ketamine therapy.