For cancer patients undergoing chemotherapy, it’s common to experience “chemobrain” during or after cancer treatment. There are a variety of ways to treat and prevent chemobrain, but first — what is chemobrain?
What is chemobrain?
Chemobrain is a mental fogginess or clouding, also referred to as brain fog, chemofog, or Postcancer Cognitive Impairment (PCCI). It can be caused by surgery and radiation as well, but it usually more pronounced if you’ve had chemotherapy. Chemobrain is a cognitive impairment limiting mental clarity; it can affect short-term memory, attention span, concentration, multitasking, and word finding. The severity and symptoms of chemobrain can vary between individuals, so it may be a good idea for patients experiencing chemobrain to have neuropsychological testing. This helps to get a full picture of your cognitive functioning and can be useful for receiving accommodations at school or work if needed.
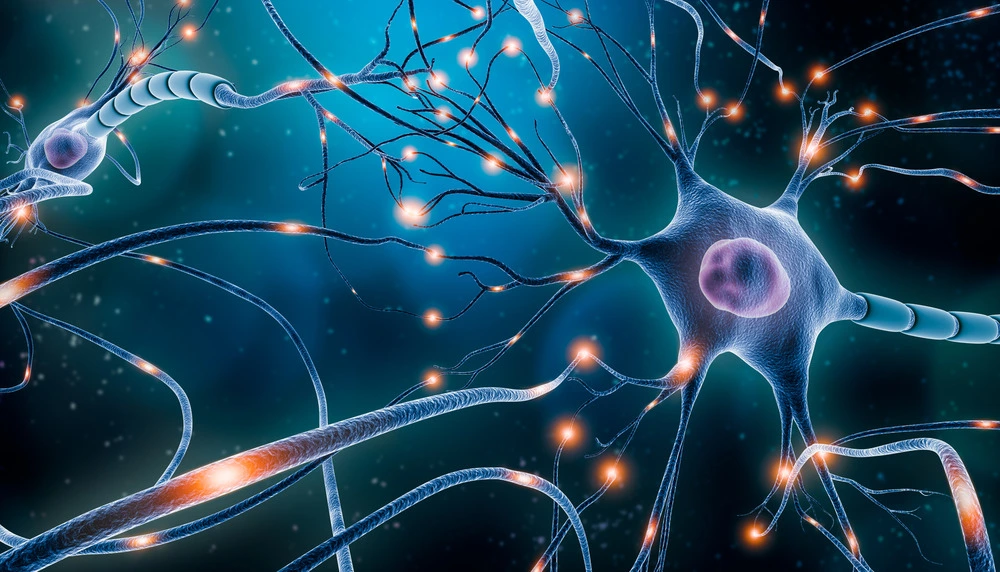
Chemobrain is in part based on mind and body fatigue; some animal studies have shown a temporary reduction in brain cell growth in key areas that control memory and learning caused by chemotherapy. In general, 17-35% of cancer survivors experience chemobrain after treatment has ended. Some of the pathways have yet to be illuminated, but we do have a general idea of what is going. Brain Derived Neurotrophic Factor (BDNF), a protein that enables the growth, proliferation, and plasticity of new neurons is limited by chemotherapy drugs, which affects mood, cognition, and memory severely. Multiple functional neuroimaging studies, mostly using fMRI, have shown impaired processing and activation of the prefrontal cortex, which leads to limited attention and ability to focus.
Do all chemotherapy patients get chemobrain? Does it ever go away?
Research shows that approximately two-thirds of chemo patients report cognitive issues. Genetic factors can increase the risk of developing chemobrain; women may be more at risk than men.
For almost all patients, chemobrain symptoms improve in 9-12 months after chemotherapy completion. It is common to still have symptoms six months after chemotherapy. A small percentage of patients may have longer term effects of chemobrain, that can be noticeable even 10 years after treatment. Long term effects, however, should remain stable. If symptoms worsen this long after treatment, seek medical attention.
How is chemobrain treated?
One of the best ways to alleviate and prevent chemobrain symptoms is regular exercise. Aerobic exercises have been determined as the most effective for this — this includes exercises like running, swimming, cycling, or dancing. It’s also important to check your thyroid and vitamin D and B12 levels, and make sure you’re being treated for any sleep problems, anxiety, or depression. Playing brain games or practicing brain exercises is another great natural way to reduce the symptoms of chemobrain. Of course, medications are oftentimes used as well, with sunitinib and methylphenidate both showing general favorable results for treating chemobrain. Additionally, neurofeedback has been shown to increase cognition in those suffering from chemobrain up to 5 years post-treatment.
Transcranial magnetic stimulation is another treatment option for brain fog caused by chemotherapy. Bespoke Treatment offers TMS treatment for chemobrain. As TMS alters neural activity in targeted areas, it has already been tested in models of aging and neurodegenerative diseases and has been shown to slow or prevent the reduction of neurogenesis and gliogenesis (the generation of new brain cells). This indicates that TMS could be effective at promoting neural creation in key cognitive areas and preserving cognitive function. TMS is a great treatment for chemobrain because it both increases BDNF, which has been reduced from chemotherapy, and directly increases activity in the prefrontal cortex, which has also been impaired from chemotherapy.
TMS is a noninvasive procedure that sends repeated magnetic pulses into the brain in order to stimulate neurons in a specified area. It is commonly used as a treatment for depression, but is also used to treat a variety of conditions, including anxiety, PTSD, OCD, and chronic pain. TMS is safe and low-risk, with most common reported side effects being a mild headache or lightheadedness that dissipates shortly after treatment. Find out if you’re eligible for TMS treatment today.