PTSD, or post-traumatic stress disorder, is a mental disorder that is sometimes experienced after an individual experiences or witnesses a traumatic event. It is often significantly debilitating, and symptoms can consist of flashbacks, nightmares, and unwanted thoughts, avoidance of thoughts or reminders of the event, severe emotional distress in response to thinking about the event, as well as other negative emotional and physical changes such as depression, anxiety, irritability or being easily startled, trouble sleeping, and difficulty maintaining relationships. PTSD is most common among war veterans; studies show that PTSD rates vary from about 10-30% among veteran populations.
Established psychotherapies such as prolonged exposure therapy (PE) and cognitive processing therapy (CPT) are effective for treating PTSD among veterans, however many individuals have trouble completing therapies. Additionally, although therapy may reduce symptoms, approximately two-thirds of patients still meet PTSD criteria after completing therapy.
Cognitive processing therapy involves elements of exposure combined with cognitive therapy; patients confront their maladaptive beliefs and conflicts associated with memories of the traumatic event, ultimately developing alternative views of the trauma that are more realistic and balanced. While CPT was originally developed for victims of sexual assault, there have been revisions specifically designed for combat veterans within the VA Healthcare system.
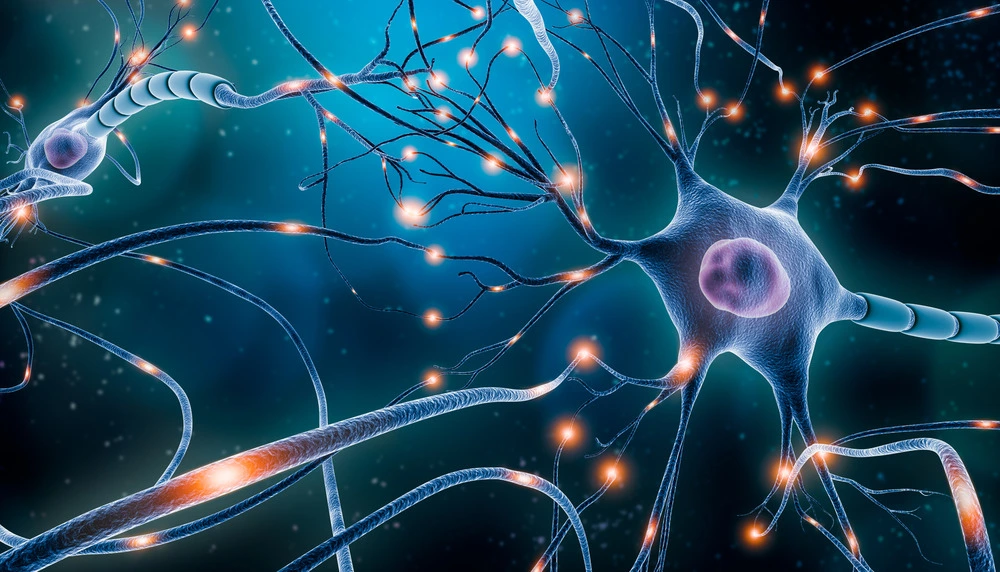
In 2018, Kozel et al. examined the efficacy of TMS in increasing the effectiveness of CPT among combat veterans of recent conflicts experiencing PTSD. Researchers conducted a randomized double blind study, giving one group real TMS before beginning CPT, and one group sham TMS. Results showed that TMS significantly augmented cognitive processing therapy.
The study participants cohttps://www.bespoketreatment.com/choosing-between-tms-therapy-and-ketamine-heres-what-you-should-know/nsisted of veterans that were deployed to combat regions in or following 2001 who were currently experiencing combat-related PTSD symptoms (with a medical diagnosis). All participants were recruited from the community via military installations, Veteran Centers, VA hospitals, and other veteran associated organizations. Participants consisted of both male and female veterans between 18 and 60 years of age.
All participants were screened and PTSD symptoms were measured using self-report and clinician rated assessments before beginning the trial. All participants meeting full criteria were randomly assigned to sham or active groups. 54 participants were assigned to the active TMS group, and 49 to the sham group. Both groups received CPT after the TMS session. Before each therapy session, a single session of rTMS was administered to the right dorsolateral prefrontal cortex, delivered at 110% of motor threshold at 1 Hz for 30 continuous minutes, totaling 1800 magnetic pulses. Sixty-minute CPT sessions were conducted immediately following rTMS treatment. Both groups received sessions one day per week and completed 12 total sessions. Measurements were conducted at baseline, after the 5th session, after the 9th session, 1 month post-treatment, 3 months post-treatment, and 6 months post-treatment.
Both groups demonstrated significant symptom improvement at all measurement points compared to the baseline. For patient-rated or self-report assessments, symptom severity was significantly reduced in the active rTMS group at all assessment periods compared to the sham rTMS group. For clinician rated assessments, symptom severity was significantly reduced in the active rTMS group at session 5, 3 months, and 6 months. The effect of TMS was weaker for clinician rated tests, but still reduced PTSD symptoms compared to sham TMS.
These results show that rTMS administered immediately before CPT helped to augment the effects of therapy and further reduce PTSD symptoms among combat veterans. Further research is needed to generalize results to other populations, but this study shows that TMS continues to be a promising treatment option for individuals with PTSD, especially as an augment to standard therapies.